Strategies on Overcoming Obstacles to Improve Specialty Pharmacy Performance
By Sean McCarthy and Ed Doran
One of the data quality challenges that we’ve been tackling here at IntegriChain is an issue that really seems to be resonating with life sciences access teams lately: data quality concerns around patient identifiers or patient mastering. We have spent a lot of our effort and focus in the last few years on capabilities related to identifying data quality issues, as well as on enrichment strategies to help our customers overcome these quality issues. Through our extensive benchmark data, we are able to uniquely identify and report on this analysis.
We think this shift in focus has a lot to do with patient journey analytics. Manufacturer access and brand teams are looking much more closely at patient service analytics and patient barriers. But in order to effectively do this, you really need to understand who your patient is.
Within the specialty pharmacy world, patients interact with so many different entities along their patient journey. This is why the journey of the patient has really become critical for manufacturers. If manufacturers tried to truly understand the performance of their network, they need a 360° view of the space. In fact, many of these manufacturers don’t realize how many patient IDs are missing in their patient data or how many patients actually have multiple patient IDs, even from the same provider. They don’t understand that the longitudinality has been broken many times for a patient. All of these are having downstream impacts; impacts on insights impacts on patient journey visibility, impacts on KPIs, and certainly impacts on patient services.
In our experience, there are four unique situations where people are time and again encountering issues that create patient mastering problems and challenges. There are more that we can think of, but these four are very symbolic, as they represent a lot of what people are experiencing and have been experiencing with patients with patient mastering IDs. We’ll discuss these four challenge cases and then discuss five strategies for overcoming these obstacles.
The Four Challenge Cases:
Null or Missing Patient Identifier
Challenge: Manufacturers will receive patient status records without patient identifiers.
This is probably the most straightforward patient master challenge that manufacturers actually encounter, and it’s a lot more common than you think. A quick analysis that we performed on some data sets found that 5% of patient status records were missing key identifiers, which is quite honestly higher than we thought it would have been.
It’s an interesting stat because most people would think that during the initiation, the new referral phase for a patient is when we would be missing this, but that’s not always the case. What will often happen is during the patient journey, these records will get lost and won’t be carried from system to system. There’s different reasons for this, but most of our manufacturer customers have processes that really just take into account the last reported ID.
A good example of this is if you had four patient status records that were updated all with a patient identifier, and the fifth was empty or null. It’s the fifth that will be processed and used. There’s no concept of mastering it. There’s no concept of, “Oh, I know who this is. I’ve received identifiers four times. I’m going to take that into account and fill in that null or void.” Most manufacturers won’t.
We’ve seen this impact where a patient won’t get a welcome kit if they have a missing ID. We’ve seen FRM teams not engaged because the system drops them off as a null identifiers. It can also create all sorts of issues or habits around patient identification.

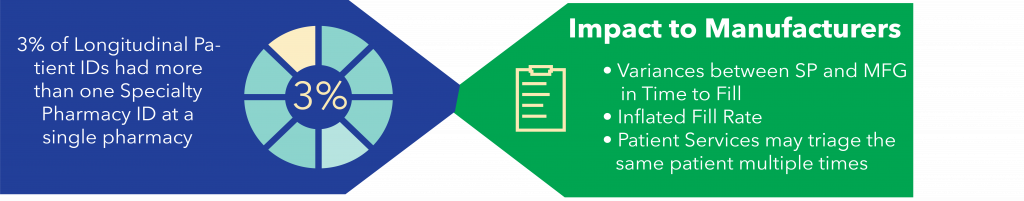
Two SP IDs for one Longitudinal ID
Challenge: Manufacturers will receive patient status records where a single patient will have multiple Specialty Pharmacy IDs
In this case, a patient seeking therapy will first be written a script and referred to a specialty pharmacy. Once the patient has been referred, the specialty pharmacy will engage the patient and collect some initial information about them. It is here where the specialty pharmacy will create the first specialty pharmacy patient ID for that patient. Once data about this interaction has been sent to a data aggregator like IntegriChain, a longitudinal patient ID is also created for that patient.
A few days later, the specialty pharmacy will re-engage the patient and continue the process of initiating them onto therapy. It is during these follow-up steps where a second specialty pharmacy ID might be generated and it can happen for a variety of reasons. The specialty pharmacy might collect new information about the patient; they might have transferred internally to another branch location that uses a different pharmacy system, or some process within the first engagement of the patient was executed incorrectly, and the patient needs to be re-initiated.
There are several other examples of why a new specialty pharmacy patient ID might be generated, but the key takeaway here is that a new identifier has been created for the patient within the same specialty pharmacy. When the specialty pharmacy sends reports of additional status data about the patient to the data aggregator, the aggregator still identifies that patient with the same longitudinal patient ID that was originally created when the first statuses were reported a few days prior.
When IntegriChain investigated the scenario, we found that about three of all longitudinal patient IDs had more than one specialty pharmacy patient ID within a single specialty pharmacy. While 3% may seem small, this can still have an impact on key performance indicators that the manufacturers and specialty pharmacies use to communicate about how effective they are at supporting their patients.
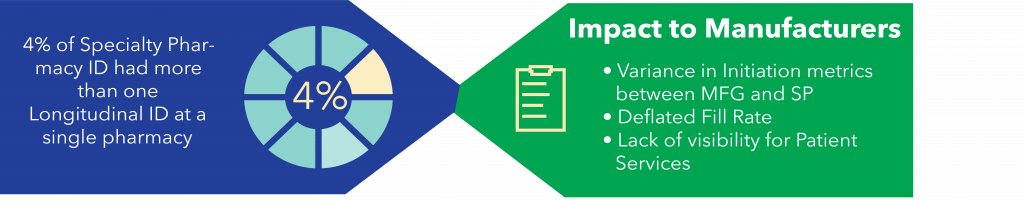
Two Longitudinal IDs for one SP ID
Challenge: Manufacturers will receive patient status records where a single patient will have multiple Longitudinal IDs
Here, a patient seeking therapy will first be written a script by their healthcare provider and referred to a specialty pharmacy. Once referred, the specialty pharmacy will engage them and collect some initial information about them. Again, it is here where the specialty pharmacy will create the first specialty pharmacy patient ID for that patient. Once the data about this interaction has been sent to the data aggregator, that longitudinal ID is created for the patient.
In this scenario, a few days later, the specialty pharmacy reengages with the patient and discovers that some of the protected health information that they’ve collected about that patient was incorrectly entered into their pharmacy systems. Whether it be the patient’s first or last name was spelled incorrectly, their date of birth is wrong, or maybe their address has changed, the key takeaway here is that some basic information about the patient has changed.
When this information is updated and sent to the data aggregator, the aggregator sees this new information about the patient and creates a new longitudinal patient ID for a patient that’s already been reported. Data aggregators rely on the patient’s protected health information to be consistent, so when there are changes, this will often lead to a new longitudinal patient ID being created.
When we investigated this particular scenario, we found that about 4% of all specialty pharmacy patients IDs at a specific pharmacy had more than one longitudinal patient ID associated with it. Again, while 4% may seem small, this can have a very similar impact on key performance indicators that manufacturers and specialty pharmacies use to communicate about how effective they are at supporting their patients.
Two Longitudinal IDs due to Hub and or SP Transfer
Challenge: Manufacturers will receive patient status records where a single patient will have multiple longitudinal IDs for transferred patients
This is probably the most complex and the largest issue we’ve seen in the industry. Very similar to our last two use cases, the initial phase of the patient journey for patients who transferred is very similar to the previous challenge cases I just described. Patients are referred to either a hub or a specialty pharmacy to start their journey, and some initial information is collected about the patient.
Once the hub completes the reimbursement support or the first specialty pharmacy identifies they will not be able to support the patient, both parties will transfer a patient to a new pharmacy to be initiated and supported on therapy. While each entity will have their own unique identifier for the patient, the idea is that the data aggregator will be able to use the patient’s protected health information to identify the patient as the same person moving between the hub and each specialty pharmacy. This gives the manufacturer key insights into where patients are and who needs the most support. However, each entity might collect protected health information about the patient differently causing variances in key information like first and last name, date of birth, or address of the patient. When this happens, the data aggregator will create a new longitudinal patient ID for the same patient as they move from the hub to the specialty pharmacy or from one specialty pharmacy to another.
You might wonder: How often does this really happen? During our investigation, IntegriChain found that a little over 19% of all patients who are transferred, either from a hub to a specialty pharmacy, or between two specialty pharmacies, were never re-identified after being transferred. That’s a pretty big number. It’s clear that this issue will have a dramatic impact on the manufacturer’s ability to support patients as they move through their specialty pharmacy network.
Without visibility into these patients, the manufacturer will be unable to deploy resources, to help triage patients who have transferred. This creates a big risk for patients that try to initiate therapy as they’ve essentially been lost in the shuffle.

Strategies for Overcoming These Obstacles
Advance Data Quality Checks
While this is surprisingly not standard practice for many data aggregators, a majority of these mastering issues can be easily detected with advanced analytics and should be a part of your data stewardship process. It is a part of IntegriChain’s Data Quality Cockpit, as we firmly believe that detecting issues can not only lead to correcting the issue but can also help identify emerging patterns.
Data Lineage
This is about the concept of tracking or passing patient identification information, almost from one provider to another. A lot of manufacturers don’t even have the concept of all these IDs in their data model, and they certainly don’t utilize it from passing from one to the other when doing longitudinality or when calculating IDs.
Secondary Matching Process
This is really talking about matching, especially post-transfer. This is when patients actually go to the hub and disappear. A new patient of course appears in another specialty pharmacy with a different longitudinal ID in a different specialty pharmacy ID, but you don’t know. There’s no connection.
That’s why IntegriChain is starting to deploy secondary matching processes and hunting for commonalities across payers and channels in each HCPs, and maybe PHI that’s been allowed to be utilized. We’re seeing great success reconnecting these patients and reducing that 19% margin.
Machine Learning Techniques – Pattern Detection
Here we’re deploying some supervised machine learning in a neural network and hunting for patterns of patient mastering issues. We’re actually trying to predict them and the patient journey scenarios and patient mastering issues. This learning model really helps us to call them out. It not only helps us to identify them, but also helps us to call it out and to coach our specialty pharmacies on the issue.
Coaching Best Practices
This is probably one of the most important things you can do, and it’s interesting how a lot of manufacturers aren’t doing this. A lot of patient mastering issues are caused by how patient information is gathered, how it’s entered, how it’s submitted, how secondary systems are submitted. Some manufacturers don’t even have insight into the clinical systems that are recording this, whether it’s a subsidiary of the one or there’s multiple subsidiaries. Are there internal transfers that are happening? A lot of things are being created because of those issues.
The more they know about it and the more they can coach for consistency for their brand, the more that they can coach the handoffs and the understanding between specialty pharmacy providers and how to record this, the better the results will be. We’ve seen some manufacturers use either an advanced service or have actually intervened with their own best practices of how they’d like specialty pharmacies to enter this information and have achieved amazing results.
Interested in learning more? Watch a webinar replay on this topic, “Overcoming the Patient Data Mastering Challenge to Improve Specialty Pharmacy Performance” >







